Jan 04, 2026·7 min
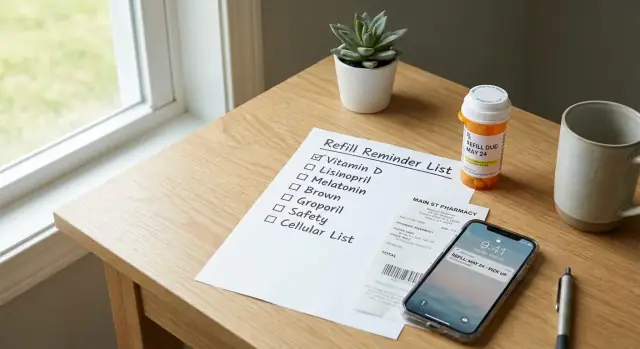
Medication refill reminder list to avoid running out
Build a medication refill reminder list to track refill dates, pharmacy numbers, and pickup plans so you can avoid last minute gaps and missed doses.
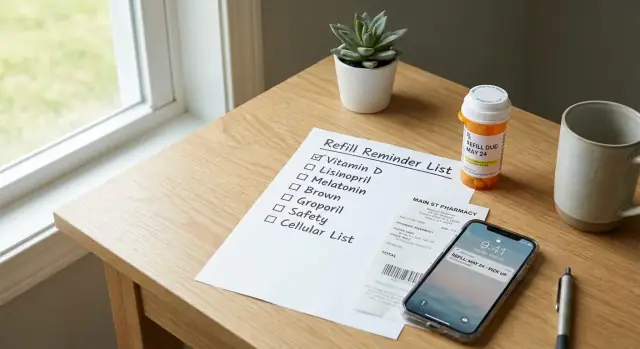
Build a medication refill reminder list to track refill dates, pharmacy numbers, and pickup plans so you can avoid last minute gaps and missed doses.
Running out rarely feels dramatic until it happens. It looks like noticing on a Friday night that you only have two pills left, or remembering on Sunday that the pharmacy closes early. It also happens when you travel, stay at someone else’s place, or have a busy week and stop looking at the bottle.
Refills are easy to misjudge because the math isn’t always clean. You might start a medication a few days after you picked it up, skip a dose, take an extra “as needed” dose, or get new directions from your clinician. Some pharmacies need time to order stock. Some prescriptions require approval before they can be refilled. Even when you do everything right, the process can still take a few days.
A medication refill reminder list reduces surprises. The goal is practical: notice low supply earlier, know who to call, and get the refill moving before you’re down to the last dose. With a simple system, refills feel like routine instead of an emergency.
This is organization help, not medical advice. Always follow your prescriber’s instructions, and ask your pharmacist or clinician if you’re unsure about timing, early refills, dose changes, or what to do if you miss doses.
This kind of list helps most when:
A common scenario: you have a refill date in your head, but the pharmacy needs a day to request approval, and your doctor’s office is closed over the weekend. A simple list with refill dates and pharmacy phone numbers turns that into a quick check and an earlier call, instead of a stressful gap.
A good medication refill reminder list is short enough to update, but detailed enough that you (or a helper) can act fast. The aim is one place where you can see what you take and who to contact.
Start with the details that most often cause delays. If you’re missing even one of these, you can end up searching while you’re already low.
Write it in plain language so it’s usable under stress. Example: “Metformin (sugar med) 500 mg, 2x/day, Pharmacy: Main Street, (555) 123-4567, Rx #123456, Dr. Patel.”
A single “notes” line can save time later. Use it for things like whether it’s mail order, a typical turnaround time (“needs 2 days”), or a rule you’ve hit before (“needs doctor approval each time”).
If delays happen often, add a short backup plan, like a second pharmacy number or a reminder to ask the prescriber about an alternative if the medication is out of stock. Keep it brief so you’ll actually maintain it.
A refill date tracker works best when it’s based on dates you can trust. You only need a few details from the label, receipt, or pharmacy app.
Start with the last fill date. That’s the day the pharmacy gave you the medication (not the day you started taking it).
Next, note the days supply. This is how many days the bottle or pack is meant to last if you take it as directed.
From there, calculate your expected run-out date:
Example: You picked up a 30-day supply on April 1. If you take it daily, you expect to run out on April 30.
Now add the next refill eligible date. This is the earliest day the pharmacy or insurance will allow the next fill. Many plans allow refills a few days early, but it varies. If you’re not sure, call and ask: “What’s the next refill eligible date for this prescription?” Write the exact date down.
Even when everything goes smoothly, weekends, travel, stock delays, and approval steps can slow things down. A simple rule is to set your personal “refill start” date 5 to 7 days before the run-out date.
For each medication, one line usually covers it:
Some medications (often controlled substances) have stricter rules. Early refills may not be allowed. Pharmacies may need extra verification. Your prescriber may require a visit. For these, the buffer still matters, but be ready for the pharmacy to fill only on the eligible date. If you’re traveling, ask about options well ahead of time.
The best medication refill reminder list is the one you’ll open when you’re busy. If updating takes more than a minute, it gets skipped, and that’s when gaps happen.
Pick the place you already check daily. Some people live in their calendar. Others keep a notebook on the counter. Choose one home for refills, not three.
Whatever you choose, keep the layout consistent: one line per medication, with the same fields in the same order. That turns updates into a habit instead of a mini project.
A simple layout that works for most people:
Add one field that stops the “Did I already do this?” problem: Status.
Keep status options simple: requested, ready, picked up. If you use paper, a small checkbox next to each status is enough.
To keep updates under a minute, update at only two moments:
Set a timer for 15 minutes and aim for “good enough.” A simple list you keep using beats an ideal one you abandon.
Grab your prescription bottles/boxes (or photos of the labels), your pharmacy app (if you use one), and your calendar or reminder app.
Say you pick up a 30-day supply on April 1 and take one tablet daily. Your run-out date is around April 30. If your pharmacy usually needs two days to fill and you sometimes miss a call back, set your reminder for April 23 to 25. If it’s a controlled medication with tighter rules, set the reminder for the earliest day you’re allowed to request it.
Before the timer ends, scan for gaps. Do you have an Rx number for each item, and at least one reminder date you can act on this week? If yes, the list is ready to use.
A reminder only helps if it matches the real steps. Most refills aren’t instant: you request it, the pharmacy processes it, and then it’s ready for pickup or delivery. That’s why prescription refill reminders work best as two separate reminders, not one.
Use channels you already notice. A perfect app you never open won’t help.
For phone calls, keep a tiny script next to your pharmacy phone numbers list so you don’t have to think.
Hi, this is [Full Name], date of birth [MM/DD/YYYY].
I’m calling about a refill for prescription number [Rx #] for [Medication name].
Can you tell me if it’s ready, and what time I can pick it up?
If it’s not ready, what’s the next step and when should I check back?
If you manage multiple people or several medications, add a repeating weekly check-in (for example, every Sunday evening). Use it to scan the next two weeks, confirm which refills need requests, and make sure the right pharmacy number is saved.
Refill gaps usually happen for boring reasons. A small mismatch between what you track and what real life does can leave you short for a day or two.
One common issue is splitting key info across places. If your pharmacy phone numbers list is in your contacts, but your refill list is on paper or in a spreadsheet, you waste time when something goes wrong. Put the pharmacy number right next to each medication.
Another frequent mistake is tracking “refill due” but not “run out.” “Refill due” is a pharmacy or insurance rule. “Run out” is your actual supply. If your reminder is based only on the due date, you can still end up with two doses left and no plan.
Dose changes break systems fast. If your clinician increases your dose, your old math is wrong immediately. Update your medication refill reminder list the same day any directions change.
Automatic refills can fail quietly. Insurance pauses, out-of-stock items, a new prescription number, or a missed text message can all stop a refill from going through. Treat auto-refill as helpful, not guaranteed.
Timing details matter, too: travel, holidays, and pharmacy hours. A Sunday run-out date isn’t the same as a Friday run-out date.
Most gaps are prevented with a few habits:
Example: If you leave town Thursday night and your pharmacy closes early on Fridays, a refill you planned for Friday can turn into a missed weekend dose unless you move the reminder to Tuesday or Wednesday.
Do a fast “stress test” on your medication refill reminder list. The point is to catch missing details before they turn into last-minute surprises.
Start with contact info. A reminder is only useful if you can act quickly. Make sure you have at least one correct pharmacy phone number saved and clearly labeled. If you use more than one pharmacy, note which medications go where.
Next, verify that every regular medication has a real run-out date written down. “Sometime next week” is where gaps happen. If the bottle says 30 tablets and you take one daily, the run-out date should match that math. If your dosing varies, add a note so your future self understands why the date can shift.
Now check timing. A common sweet spot is 5 to 7 days before run-out. That gives time for delays, insurance checks, and weekends. If you use mail order, you may need 10 to 14 days.
Two-minute pass/fail check:
For medications with special rules, add a short label like “PA may be needed” or “controlled, early refill limits.” That prevents you from assuming a refill will be instant.
Maya takes two daily meds (a blood pressure tablet and an antidepressant) and keeps a rescue inhaler for asthma. She’s leaving Saturday morning for a two-day family trip. In the past, she noticed an empty bottle on Friday night and had to call the pharmacy right before closing.
This week, she uses a medication refill reminder list that sits where she keeps her meds. On Monday, she checks what she has left and writes down three things for each medication: pill count, last fill date, and the pharmacy phone number.
By Tuesday, her refill date tracker shows a problem: the blood pressure medication will run out on Sunday, right in the middle of the trip. She calls during lunch and marks the refill as Requested (Tue 12:15 pm).
On Thursday afternoon, she gets a text from the pharmacy. Before she leaves work, she updates the list to Ready (Thu 4:40 pm) and picks it up on her way home. Friday night stays quiet.
Her status notes are short and clear:
Caregiver angle: Maya’s dad checks in every Sunday. During the call, she reads the three lines out loud and mentions anything marked “requested” but not yet “ready.” It takes one minute, and it helps catch delays early.
A refill system only works if it stays current. The easiest approach is one “master” list, plus a smaller weekly view so you only look at what matters right now.
Your master list should include medication name, dose, prescriber, pharmacy phone number, typical days supply, and the next refill date (or “refill by” date). Your weekly view is just what’s due soon (the next 7 to 14 days).
A low-effort rhythm:
Decide where the list lives so you can find it quickly. Keep it in one place you already check daily (notes app, paper by where you store meds, or a shared household document). If you care for someone else, store it where a backup person can access it without guessing.
If you want more automation, you can build a simple personal tracker that stores your meds, calculates run-out dates, and prompts you to request refills. Tools like Koder.ai are designed for building web, server, or mobile apps from chat, which can be handy if you want a small React or Flutter app you can adjust over time and export the source code for.
If your week is packed, keep it simple: set a Sunday 5-minute check. Open your weekly view, request any refills due within 10 days, and update the master list right after you place the request.
Start the refill process when you’re about 5 to 7 days from running out. That buffer covers weekends, approval delays, and out-of-stock problems without making you feel like you’re constantly refilling.
Use the last fill date (when you picked it up) plus the days supply on the label. That gives you a reliable run-out estimate even if you didn’t start taking it the same day you filled it.
At minimum, record the medication name, dose and schedule, pharmacy name and phone number, Rx number, and prescriber name. Those details are what usually prevent the “I can’t refill this without more info” situation.
A single notes line is enough, like “usually takes 2 days,” “needs doctor approval,” or “mail order.” Keep it short so you’ll update it, and only add what saves you time when something goes wrong.
Use two reminders: one to request the refill and one to confirm it’s ready. This matches how refills work in real life, where processing time and issues like “too early” can appear after you submit the request.
Choose the place you already check every day, like a notes app, a calendar, or a paper sheet where you store meds. The best format is the one you’ll actually open when you’re tired or busy.
“Refill due” is a rule set by the pharmacy or insurance, while “run out” is your real supply at home. Track both, because you can be “not due yet” and still be close to empty if the timing or dosing changed.
Update your list the same day the dose changes, because your old run-out math becomes wrong immediately. If your dosing varies, add a brief note so your future self understands why the date can shift.
Treat auto-refill as helpful, not guaranteed, and still check a few days before you need it. Auto-refills can fail because of insurance pauses, stock issues, or a new prescription number, and you want time to fix that.
Yes, if you want more automation, you can build a simple personal tracker that stores your meds, calculates run-out dates, and prompts you to request refills. With a vibe-coding tool like Koder.ai, you can describe the app in chat, generate a small web or mobile tracker, and adjust it over time if your meds or routines change.